Endurance Training/Cardiorespiratory
(54) PHYSIOLOGICAL EFFECTS OF WORK-TO-RECOVERY RATIO DURING AEROBIC INTERVAL EXERCISE WITH BLOOD FLOW RESTRICTION

Jake R. VanArsdale
Student
Coastal Carolina University
Conway, South Carolina, United States- JS
John Grayson Sossamon
Student
Coastal Carolina University
Conway, South Carolina, United States - TR
Timothy R. Rotarius
Assistant Professor
Coastal Carolina University
Conway, South Carolina, United States - MD
Marcos Daou
Assistant Professor
Coastal Carolina University
Conway, South Carolina, United States - JL
Jakob D. Lauver
Associate Professor
Coastal Carolina University
Conway, South Carolina, United States - JG
Justin P. Guilkey
Associate Professor
Coastal Carolina University
Conway, South Carolina, United States
Poster Presenter(s)
Author(s)
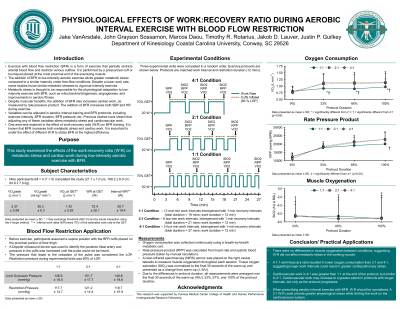
A mechanism of adaptation to aerobic exercise with blood flow restriction (BFR) is increased local metabolic stress, however, BFR can also increase cardiac work, which could be affected by the work interval-to-recovery duration ratio (W:R ratio).
Purpose: This study examined the effects of W:R ratio on metabolic stress and cardiac work during low-intensity aerobic exercise with BFR.
Methods: Participants (20.7 ± 0.8 yrs) completed a graded exercise test on a cycle ergometer to assess ventilatory threshold. On separate days, participants completed three experimental interval (INT) exercise protocols with intermittent BFR, in a random order. All protocols consisted of a 4-min warm-up ([20 W] WU), work INTs (70% work rate at ventilatory threshold), and 1-min recovery INTs (20 W) between work INTs. The work INTs in the three protocols were: 1) six 2-min INTs (2:1), 2) twelve 1-min INTs (1:1), and 3) three 4-min INTs (4:1). During work INTs, BFR cuffs rapidly inflated to 80% of limb occlusion pressure (LOP) and deflated during recovery INTs. In each protocol, the duration of work INTs and BFR was 12 min. LOP was the pressure at which the posterior tibial artery pulse ceases by Doppler auscultation. Oxygen uptake (VO2) and tissue oxygen saturation (StO2, %) were averaged over the last 30 s of INTs at 33%, 67%, and 100% of the protocol. StO2 values were reported as a change from baseline (20W) (∆BSL) and used to quantify local stress. Blood pressure was taken manually during the last 30 seconds of WU and INTS at 33%, 67%, and 100% of the protocol. Rate pressure product (RPP) was calculated from heart rate and systolic blood pressure to assess cardiac work. Due to the different protocol durations, data was compared at 0% (end of WU), 33%, 67%, and 100% of each protocol duration. A 2-way (trial x time) repeated measures ANOVA assessed differences between protocols. Significance was established if p ≤ 0.05.
Results: There were no differences in BFR pressure during the intervals (1:1 = 113.3 ± 13.8 mmHg; 2:1 = 114.0 ± 9.2 mmHg; 4:1 = 116.0 ± 18.7 mmHg. There was a significant interaction for VO2. VO2 was similar between conditions during WU (1:1 = 0.86 ± 0.18 L∙min-1; 2:1 = 0.85 ± 0.21 L∙min-1; 4:1 = 0.77 ± 0.77 L∙min-1). At each time point, VO2 was significantly lower in 1:1 (100% = 1.03 ± 0.33 L∙min-1) compared to 2:1 (100% = 1.19 ± 0.37 L∙min-1; p = 0.005), and 4:1 (100% = 1.20 ± 0.37 L∙min-1; p = 0.005). However, VO2 was similar between 2:1 (67% = 1.19 ± 0.33 L∙min-1) and 4:1 (67% = 1.20 ± 0.35 L∙min-1). There was a significant interaction for RPP. The only differences were between 1:1 and 4:1 at 67% (1:1 = 18415.5 ± 1170.1 mmHg∙BPM vs. 4:1 = 20570.33 ± 2526.6 mmHg∙BPM; p = 0.024) and 100% (1:1 = 19224.2 ± 2702.8 mmHg∙BPM vs. 4:1 = 22232.8 ± 2758.2 mmHg∙BPM; p < 0.001). RPP during 2:1 was not different from either condition (66% = 20687.2 ± 3793. mmHg∙BPM; 100% = 21609.3 ± 4474.5 mmHg∙BPM). There were no interactions (p = 0.925) or main effects for StO2 (1:1 100% = -7.5 ± 6.3 ∆BSL, 2:1 100% = -4.6 ± 4.5 ∆BSL; 4:1 100% = -4.2 ± 5.8 ∆BSL). CONCLUSION: W:R ratio did not affect metabolic stress. However, greater W:R ratios resulted in a higher VO2 but the highest W:R ratio increased cardiac work. The 2:1 produced higher VO2 and similar metabolic stress while limiting cardiac work. PRACTICAL APPLICATION: When prescribing aerobic interval exercise with BFR, the W:R ratio should be considered and a 2:1 ratio could give the optimal benefits.
Acknowledgements: None
